Story and photos by Darl DeVault
While Oklahoma seniors have been the most vulnerable to COVID-19, our modern heroes, medical health professionals, have also been impacted by this huge stress event.
Medical outcomes are stark. There are no proven therapies to treat or cure the disease. In Oklahoma, the vast majority of COVID-19 deaths are in seniors 65 or older, as high as 80 percent. The statistics go on and on, unchanging in dire descriptions of how vulnerable aging bodies are to the pandemic.
Another group shares a vulnerability every bit as brutal in descriptions. Our medical health professionals are the next highest death rate in America. Besides the brutal numbers of deaths, there is another facet of their suffering.
They are repeatedly exposed to preventable unmanageable stress. This immersion in the onslaught of a pandemic has the potential to inflict post- traumatic stress disorder.
In honor of the 200th birth anniversary of Florence Nightingale, the World Health Organization (WHO) has designated 2020 as the “Year of the Nurse and Midwife.” Since National Nurses Week is celebrated soon from May 6 through May 12 it is appropriate to ask one “What are you going through?”
Nurse Beth Bierig said last week from New Jersey, “Working on a floor of all COVID-19 positive patients whose change in status happens quickly without warning, makes you feel constantly guarded as to when your own medical health will quickly turn badly as well. You don’t have time to even comprehend how scary the silent killer surrounds every piece of air you work in, but it weighs heavily on your mind.”
Bierig, from Hackensack University Medical Center, goes on to explain how having a servant’s heart can put a nurse in harm’s way. “While performing life sustaining measures on your patients and respiratory fragments flood the air in the process, you can’t help but wonder, will it be saving their life that takes mine?” she said. “I don’t know the effects it will have on myself or other people, because everyone has had different experiences. Every nursing specialty has their own traumas and people are generally drawn to what they can handle.”
Also, “the support nurses receive after this will affect their long-term mental health pertaining to this situation. The whole situation has affected everyone strongly, not only health care providers. We’re living in a historic time and hopefully we all learn from it.”
From the respiratory therapists who manage ventilators, and technicians that manage ICU equipment to the direct caregivers, stress can be overwhelming. The heroes who share their servant’s heart signed up to be properly supported and use their knowledge and ability to affect positive change. Again, at present, there are no proven therapies to cure COVID-19.
Some health care professionals function where they are overwhelmed by the sheer number of deaths that take place right in front of them. Sometimes as often as hourly, these deaths may inflict a PTSD future on the frontlines of medicine.
For those healers who were constantly worried about their own health because of a shortage of personal protective equipment life can change. Just the apprehension of spreading the disease to their family could have a dire outcome.
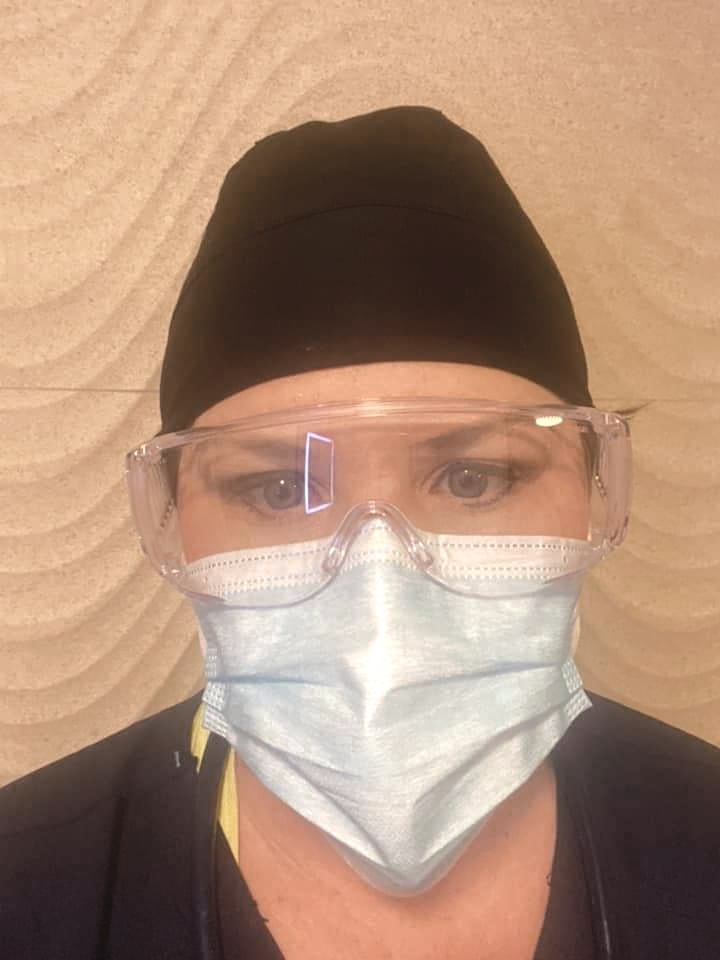
COVID-19, the severe respiratory illness caused by the novel coronavirus pandemic is extremely transmissible. Properly protected ICU critical care team workers being readied for patient interaction look like preflight prep before blastoff for our moon missions.
These heroes may share an almost as strong an impact as the vulnerable seniors who perished. Some may suffer grave symptoms of psychological stress impacting their ability to deliver medical health care in the future.
Every psyche is different in the many roles played by helping healers who suited up to sustain the COVID-19 patients. Science tells us women are twice as likely to suffer PTSD symptoms.
This pandemic is something different. The onslaught of stress can change brain wiring for the worse — at the level to create PTSD. Later, some may seek to stay away from the situations that remind them of the traumatic events.
Some caregivers may not be able to adaptively overcome the stress and adversity while maintaining normal psychological and physical functioning.
The potential for PTSD is when an individual is placed in a situation where they do not have all the needed equipment, weaponry, support by colleagues in numbers needed, or proper support from superiors. This is also fueled when they feel they do not have the proper protective material and are forced to go in harm’s way relentlessly when they fear for their own survival. On April 3, Oklahoma showed 10.6 percent of its confirmed cases were health care workers.
Situationally produced and yet self-imposed is the stress of sleeping in their cars in their hospital parking lot because they do not want to bring potential illness and death home to their families. This can result in the development of PTSD, depression and other psychiatric disorders.
In a medical scenario where our heroes ran toward the danger and healing is supposed to take place that sounds extremely abrupt. But in many of our hospitals that were overwhelmed by COVID-19 patients presenting repeated unmanageable stressors, that is exactly what was happening.
Often nurses and doctors in COVID-19 hotspots made life and death choices, deciding who was to live and who was to die because of a limited number of ventilators and limited ability to intubate. And there was the randomness of patients dying right in front of them as these patients first entered the hospital.
We must be honest. Nurses and doctors are human and cannot escape that negative impact. People who signed up to work around the sick also take great pride in learning all the ways to be healers.
To suddenly be immersed in the onslaught of hourly and daily negative scenario can have a permanently deleterious effect on the human psyche. It remains to be seen if overwhelming the individual at a high morbidity level has a lasting effect. We know brainwave activity that negativity establishes can create specific pathways in the brain that were not there before.
How do we know what effect this has on these brave people’s body and spirit when these pathways are never compensated for? These individuals may have anxiety and depression from these days forward.
The wild card in all of this are brave medical health professionals who contracted COVID-19 themselves, while trying their best to help others. Hundreds have died around the world. Yes, they signed up for this profession, but not to suffer the same as their patients.
Another stressor is some hospitals, such as the University of Oklahoma Medical Center, are cutting pay and hours because of the strict emphasis on COVID-19 leaving them cash poor.
“A grateful nation will likely create a fund offering therapy and treatment for front line medical professionals who have health problems traceable to saving lives similar to the federal World Trade Center Health Program,” Oklahoman Kara De La Pena, APRN, said. “Considering for many of us who took on preventable risks, the James Zadroga 9/11 Health and Compensation Act of 2010 will be held up as a model for providing us medical treatment. That program is funded through 2090 now.”
The seniors saved and whole world thank our heroes and seek restorative insight into the medical outcomes thrust upon the healers who fight to keep people alive.